Boost collection speeds, increase revenue, and improve operational efficiency by reaching patients on their preferred communication channel at the right time.
Patient-first, automated medical billing cycles
No more manual statement reviews or time spent preparing batch billing.
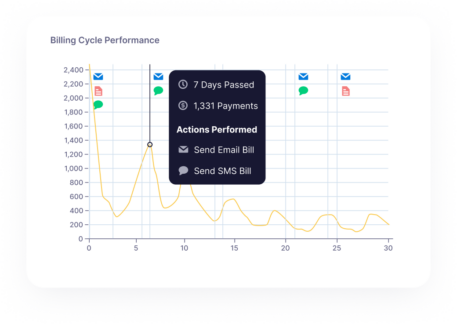
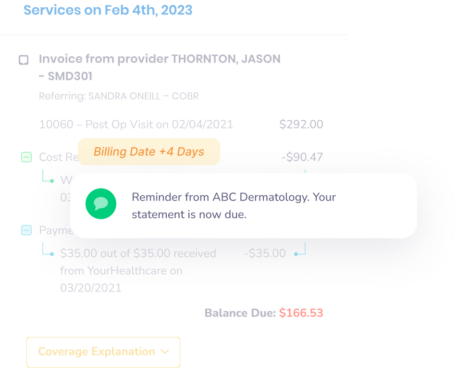
Increase collection speeds by reaching patients on the right channel, at the right time, with the right message. Inbox Health’s data-based billing cycles adapt and automate follow-up communication based on how patients interact with previous paper, text, or email messages.
Communicate on modern channels at the right time.
Timing is critical when it comes to post-visit financial patient engagement – the sooner statements are sent, the faster balances are paid. Statements are triggered to send through patients preferred communication channels via SMS, email, or paper mail. Send timely payment reminders and improve patient engagement with clear and accessible communication.
Optimize your billing team’s time.
Automated follow-up communications allow your billing team to focus on patient care and complex insurance claims instead of spending time on the phone tracking down unpaid balances.
How it works:
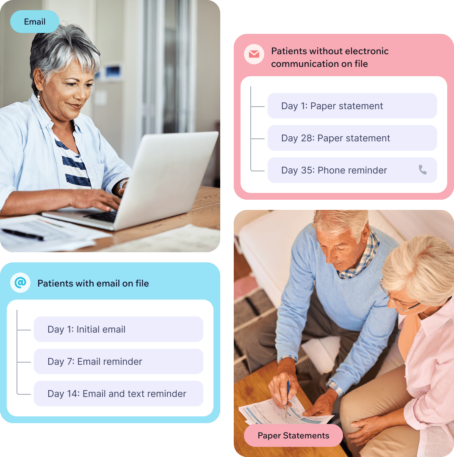
Send statements via email, text, mail, or a combination of all three. Here is an example of a billing cycle starting with each communication channel:



Real results in the first 30 days:**
-
88 %
increase in collection speeds
-
97 %
adoption rate of digital payments and communication increase in collection speeds in the first 60 pays
-
47 %
reduction in time spent managing patient A/R, resulting in lower adminstrative costs
Patient billing is personal. Let our recommended medical billing cycle get to work, or customize communications to meet your patients’ needs
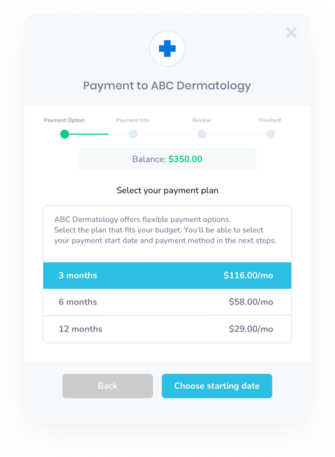
Offer payment plans
At any point in the patient billing cycle, you have the option to offer a payment plan. Billing teams also have the ability to set parameters around payment plans, determining who is eligible, when it is offered in the billing cycle, and over what period of time until the bill must be paid in full.
For example, a billing team can offer a payment plan to a patient if the total balance is over $500, after he received two bills and logged into the system to view their balance, and set the outstanding balance to be paid within six months. An alternative example is billing teams can offer payment plans to all patients after their second bill.
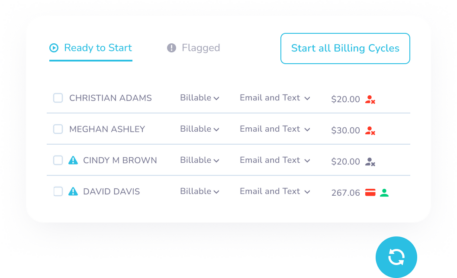
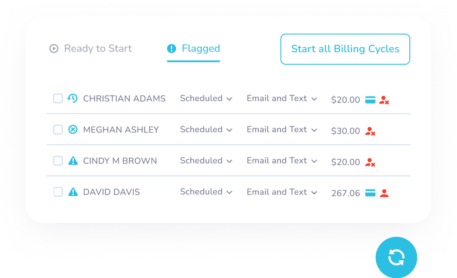
Flag actions for review
Select criteria to flag a patient for review before a billing cycle begins. This is commonly used for specific insurance payers (Medicare/Medicaid), high balances, account types, service codes, and payment reason codes.
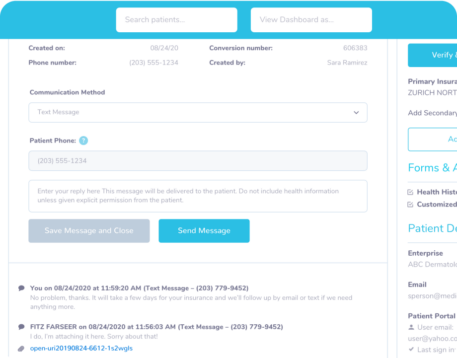
Customize your message
Inbox Health provides recommendations for your email, text, and paper messaging, but you also have the ability to edit as you see fit, down to the body copy, subject line, or emojis. You can even preview messages before you press send, so you’ll know exactly how messages appear to patients.
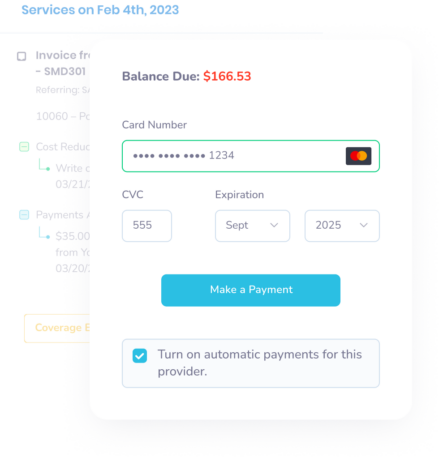
Turn on automatic payments
Increase collections speeds and revenue and eliminate delays with auto-charge. Automatic payments allow patients to save a card on file and set up recurring payments through a secure, mobile-friendly interface, which encourages on-time collections.
Get started with Inbox Health today
Inbox Health was built for medical billers. Click below and schedule a quick chat – let’s get to know each other.
FAQ
-
How does Inbox Health automate the patient billing process?
Inbox Health streamlines the patient billing lifecycle through intelligent workflows. After insurance claim adjudication, the platform automatically delivers personalized statements via email, text, or paper mail based on patient preferences, with billing cycles that adapt to patient interactions and preferences. Inbox Health automatically flags potential errors during statement review using customizable parameters and posts all payments—including paper checks—directly to practice management systems. This automation eliminates manual processes and paper-based workflows, freeing billing teams to focus on complex insurance claims and patient care.
Show more -
Can patients set up automatic payments or payment plans?
Yes, Inbox Health offers flexible payment options designed to accommodate patient preferences and financial situations. Patients can easily enroll in payment plans directly through the secure online patient portal, with billing teams having control over eligibility criteria, when plans are offered in the billing cycle, and maximum payment timeframes. The platform also supports automatic payments, where patients can save a card on file and opt to have their cards charged automatically for future bills. This option can be included in the initial communication (email, text, or paper bill). Additionally, the platform allows patients to save credit card information for future use, making subsequent payments seamless. These flexible payment options remove barriers to payment while giving patients more control over their healthcare finances.
Show more -
Is the payment system secure and HIPAA-compliant?
Inbox Health maintains robust security standards and is fully compliant with healthcare industry regulations. The platform is HIPAA-compliant, providing a secure environment for processing, maintaining, and storing protected health information. It regularly undergoes PCI DSS (Payment Card Industry Data Security Standard) assessments for handling credit card information and holds SOC 2 certification, which verifies the suitability and operating effectiveness of its information security controls. This comprehensive security framework ensures patient data and payment information remain protected throughout the billing process.
Show more -
How does this improve revenue and collection rates?
Inbox Health significantly improves revenue and collection rates through its transparent, accessible patient billing approach. Practices report patients pay up to 5 times faster with collection rate improvements of 60% in the first 60 days across different specialties. Most practices see substantial revenue increases within 30 days of implementation. Digital adoption rates consistently reach 96-100%, demonstrating strong patient preference for electronic statements and payment options. Administrative costs decrease dramatically through reduced paper statements and lower phone call volume (up to 90% reduction). This combination of faster payments, higher collection rates, and lower operational costs delivers a substantial positive impact on practice revenue and efficiency.
Show more